Glycated hemoglobin for the diagnosis and follow-up of diabetes mellitus
Author: Lina Marcela Restrepo Giraldo.
Endocrinologist. Chief of Clinical Liaison, Clinical Hematological Laboratory.
Date of publication: 19/01/2023
Glycated hemoglobin, also known as glycohemoglobin, hemoglobin A1C, HbA1c or A1C, is a special component of blood that is formed from the union between hemoglobin A (HbA), the protein found in red blood cells to transport oxygen to all tissues and cells, and some sugars, especially glucose, that enter the blood circulation after having been ingested in food (Figure 1).
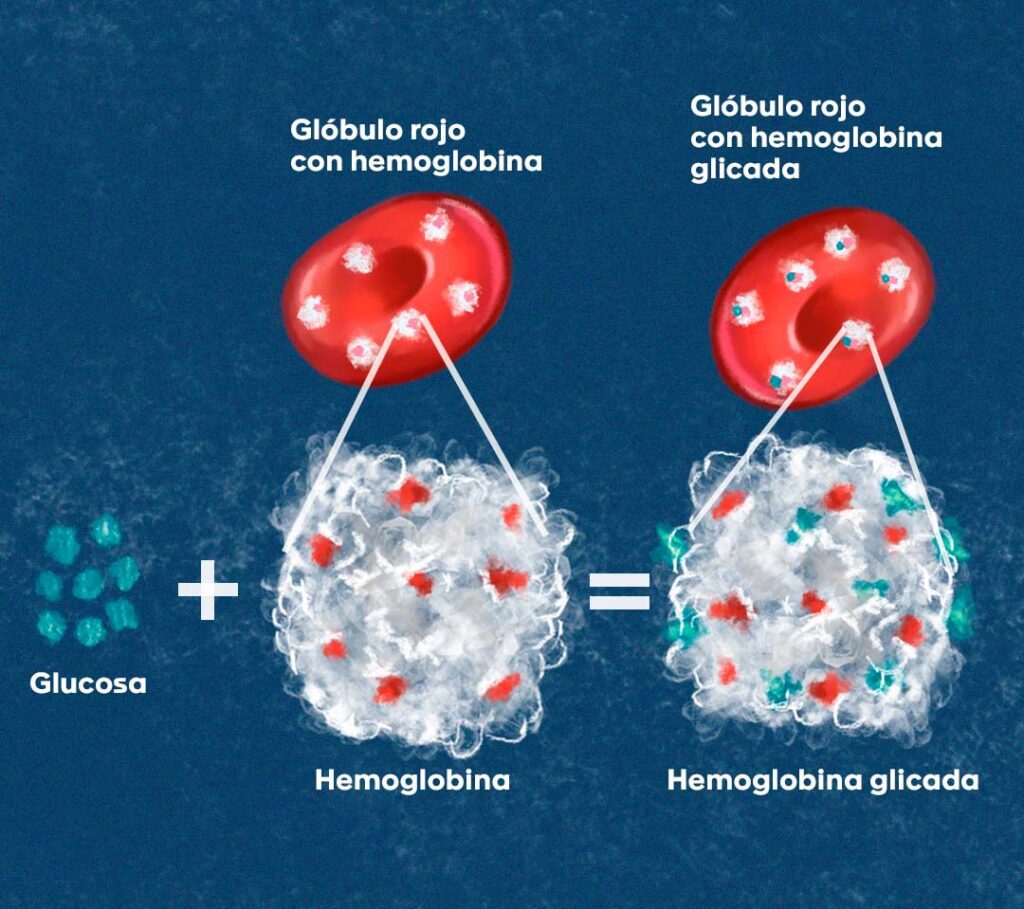
Figura 1. La glucosa se une a la hemoglobina que se encuentra en los glóbulos rojos, y que transporta cuatro moléculas de oxígeno que están unidas al hierro en su interior. Esto da como resultado la formación de la hemoglobina glicada, es decir, una hemoglobina con moléculas de glucosa adheridas permanentemente a su superficie.
The formation of HbA1c is a normal process, but the amount in which it is produced is proportional to the blood glucose levels averaged over the last three months; the estimated time that red blood cells live in the circulation. Thus, the Hb1Ac test calculates the percentage of red blood cells, with hemoglobin bound to glucose, present in the blood at the time the test is performed. Diabetes mellitus (DM) is a chronic disease, in which persistently elevated blood glucose levels are found and is classified into two main categories:
- a) type 1 DM, in which there is little or no insulin, due to autoimmune destruction of the β-cells of the pancreas responsible for its production.
- b) type 2 DM, where insulin production by the β-cells is insufficient and there is resistance to its action.
Given that insulin is the hormone that helps glucose to enter the body’s cells to obtain energy, in either of these cases (type 1 or type 2 DM), glucose does not enter and, consequently, its levels in the bloodstream increase. In addition to the fact that this disease currently affects more than 500 million people (between 20 and 79 years of age) in the world, it causes serious consequences in the blood vessels, heart, kidneys, extremities, brain, nerves, eyes, immune response and can even lead to fatal outcomes if it is not adequately controlled. For this reason, for more than 30 years, different international strategies have been sought in terms of education, timely diagnosis, adequate glycemic control and treatment, in order to reduce the risk and prevent complications in those who suffer from it.
Glycated hemoglobin in diabetes mellitus
Thanks to two large clinical studies in the 1990s, the Diabetes Control and Complications Trials (DCCT) in patients with type 1 DM and the United Kingdom Prospective Diabetes Study (UKPDS) in patients with type 2 DM, HbA1c was established as an indicator of the degree of blood glucose control and the risk of chronic complications of the disease. Then, in 2010, it was confirmed as a primary criterion for diagnosing DM (using a method certified by the NGSP and standardized with the DCCT reference assay).
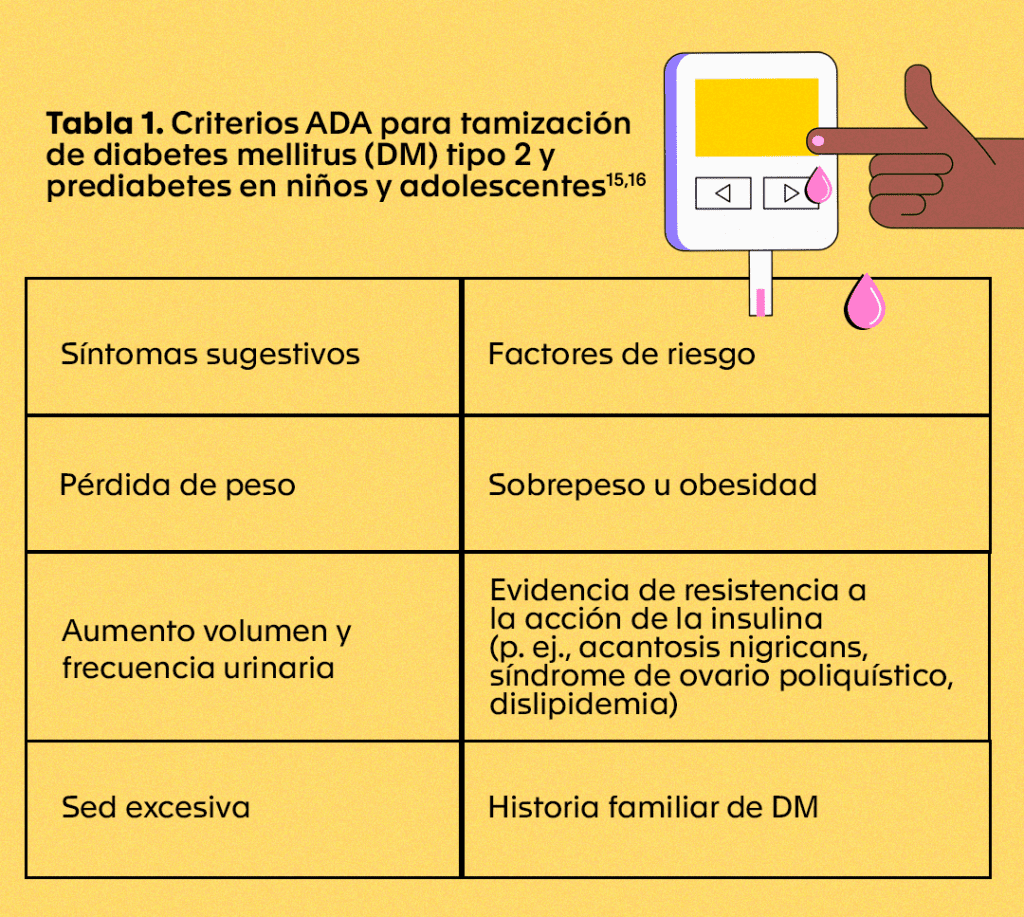
According to the American Diabetes Association (ADA) and the American College of Endocrinology (ACE), it is recommended that HbA1c levels be measured every six months in patients with stable glycemic control and at least every three months in those with variations in their glucose levels or who have changed their treatment. Routine screening for prediabetes and type 2 DM in children and adolescents is only recommended when there are suggestive symptoms and one or more risk factors (Table 1). For type 1 DM, there are still no recommendations for screening in the general population using HbA1c.
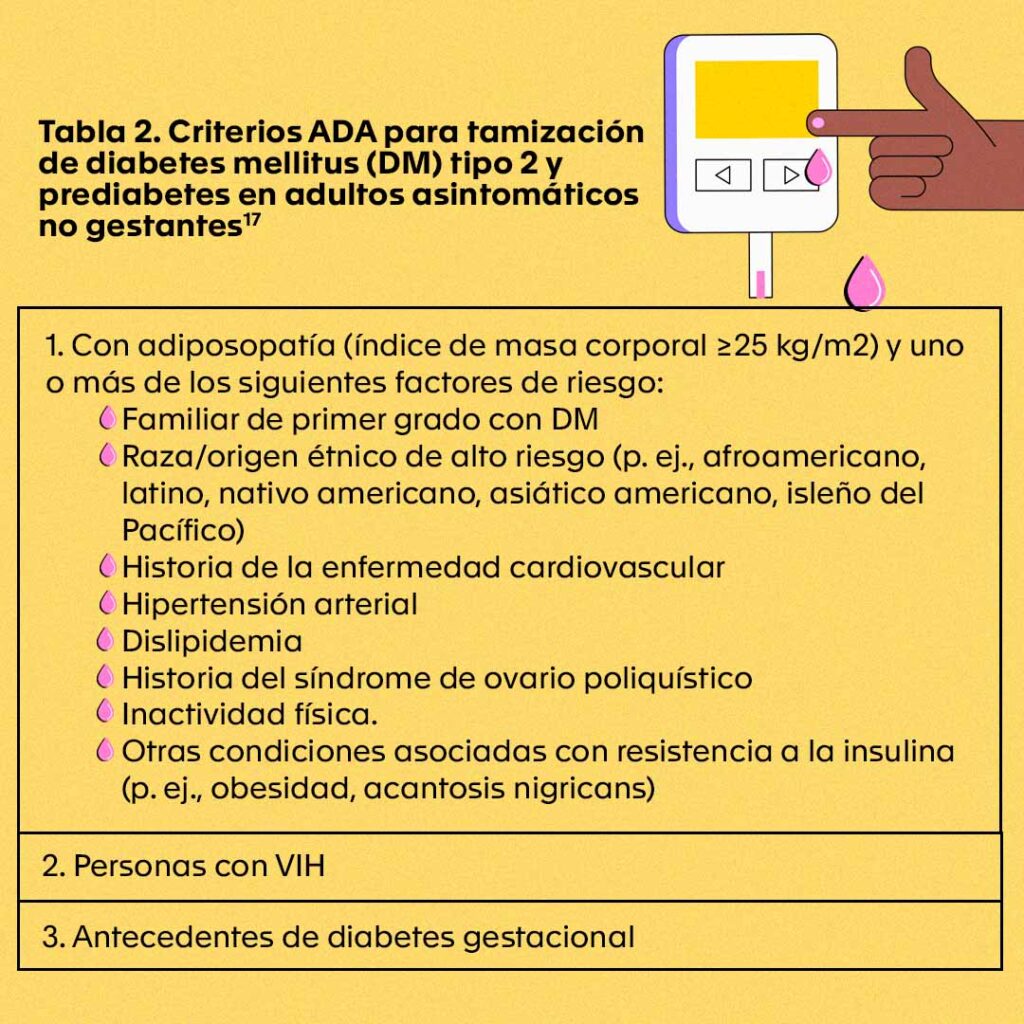
In asymptomatic adults with risk factors (Table 2), the ADA recommendation for screening for type 2 DM or prediabetes with HbA1c is to perform it every three years. For other individuals, testing should begin at the age of 35 years and if the results are normal, they should be repeated at minimum intervals of three years, considering increasing their frequency on an individualized basis according to their evolution.
Evaluation and interpretation of results
The HbA1c study requires a whole blood sample taken in a tube with EDTA anticoagulant (purple cap) which, as an additional advantage, allows it to be taken at any time of the day, without the need for fasting, and has a high stability (up to 1 week at 4 °C) until its evaluation in the laboratory. However, conditions where the half-life of red blood cells decreases, such as anemias, chronic kidney disease, pregnancy, transfusions or blood loss, etc., can lead to altered HbA1c values, so the treating physician should be aware of them when ordering and interpreting the test.
The interpretation of HbA1c results is based on pre-established values in international consensus. For example, the ADA and the ACE indicate that in order to significantly reduce DM-related complications, the goal is for adults (non-pregnant) to reach and maintain individual HbA1c values of around 6.5% and 7.0%, in the absence of low serum glucose levels (hypoglycemia). Likewise, they established for the diagnosis of DM values above or equal to 6.5%, and as a risk of developing it (prediabetes) values below 6.5%, but above or equal to 5.7%.
On the other hand, if there are discordant results between HbA1c and clinical suspicion (in the presence or absence of symptoms suggestive of hyperglycemia), the use of complementary blood glucose measurement tests (fasting blood glucose or oral glucose tolerance test) is recommended. If the two tests are concordant, the DM diagnosis is confirmed. If the two tests are discordant, the test that is above the cut-off point for diabetes should be repeated and the diagnosis is made on the basis of the confirmed test.
However, as with other laboratory results, it is important for the treating physician to consider each patient’s profile, including DM history, risk factors, type of treatment and dosage (if applicable), among others, to establish the best course of action. In addition, he/she should know the method of analysis used for HbA1c measurement and verify that the samples have been processed, preferably in a laboratory certified by the NGSP to ensure that the results are standardized and avoid misdiagnosis.
Quality-certified methods
Among the methods for measuring HbA1c there are four that are most commonly used in laboratories and accepted by the NGSP: 1) ion-exchange high-performance liquid chromatography (HPLC), which separates HbA1c from the other hemoglobin variants based on their electrical charge; And, 2) immunoassay, 3) enzyme assay, and 4) boronate affinity HPLC, which are based on structural differences between HbA1c and non-glycated forms of hemoglobin.
The optimal use of these tests and the reliability of the results they provide for the diagnosis and follow-up of DM depends on strict quality controls and standardized measurement according to the DCCT and UKPDS studies, as well as continuous monitoring of analytical performance through comparative studies with international reference laboratories such as those in the NGSP network.
In the Clinical Hematology Laboratory we have the HPLC methodology (Tosoh G8 analyzer), which measures HbA1c in an automated way, provides accurate and reliable information, and is internationally certified. In addition, we participate in the HbA1c performance evaluation programs every quarter and in the annual interlaboratory comparison tests with the NGSP, which allows us to be certified as a level I Laboratory.
To learn more about the NGSP network and the certification granted to the Hematológico click here.
To learn more about the NGSP network and the certification granted to Hematologic click here.
Bibliografía
- Eyth E, Naik R. Hemoglobin A1C. En: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK549816/
- Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomark Insights. 2016;11:95-104.
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care. 1 de enero de 2021;44(Supplement_1):S15-33.
- International Diabetes Federation. IDF Diabetes Atlas [Internet]. 10a ed. Bruselas, Bélgica: International Diabetes Federation; 2021. Disponible en: https://www.diabetesatlas.org
- Stratton IM. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 12 de agosto de 2000;321(7258):405-12.
- American Diabetes Association. 11. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes—2021. Diabetes Care. 1 de enero de 2021;44(Supplement_1):S151-67.
- Donaghue KC, Chiarelli F, Trotta D, Allgrove J, Dahl-Jorgensen K. Microvascular and macrovascular complications associated with diabetes in children and adolescents. Pediatr Diabetes. septiembre de 2009;10:195-203.
- The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. agosto de 1995;44(8):968-83.
- Introduction: Standards of Medical Care in Diabetes—2021. Diabetes Care. 1 de enero de 2021;44(Supplement_1):S1-2.
- The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N Engl J Med. 30 de septiembre de 1993;329(14):977-86.
- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet Lond Engl. 12 de septiembre de 1998;352(9131):837-53.
- The International Expert Committee. International Expert Committee Report on the Role of the A1C Assay in the Diagnosis of Diabetes. Diabetes Care. 1 de julio de 2009;32(7):1327-34.
- American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2021. Diabetes Care. 1 de enero de 2021;44(Supplement_1):S73-84.
- American Diabetes Association. 13. Children and Adolescents: Standards of Medical Care in Diabetes—2021. Diabetes Care. 1 de enero de 2021;44(Supplement_1):S180-99.
- Arslanian S, Bacha F, Grey M, Marcus MD, White NH, Zeitler P. Evaluation and Management of Youth-Onset Type 2 Diabetes: A Position Statement by the American Diabetes Association. Diabetes Care. 1 de diciembre de 2018;41(12):2648-68.
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. Introduction and Methodology: Standards of Care in Diabetes—2023. Diabetes Care. 1 de enero de 2023;46(Supplement_1):S1-4.
- Donovan L, Hartling L, Muise M, Guthrie A, Vandermeer B, Dryden DM. Screening Tests for Gestational Diabetes: A Systematic Review for the U.S. Preventive Services Task Force. Ann Intern Med. 16 de julio de 2013;159(2):115.
- Lo C, Lui M, Ranasinha S, Teede HJ, Kerr PG, Polkinghorne KR, et al. Defining the relationship between average glucose and HbA1c in patients with type 2 diabetes and chronic kidney disease. Diabetes Res Clin Pract. abril de 2014;104(1):84-91.
- Selvin E, Wang D, Matsushita K, Grams ME, Coresh J. Prognostic Implications of Single-Sample Confirmatory Testing for Undiagnosed Diabetes: A Prospective Cohort Study. Ann Intern Med. 7 de agosto de 2018;169(3):156-64.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Diabetes & Prediabetes Tests [Internet]. 2020. Disponible en: https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/diabetes/diabetes-prediabetes
- Weykamp C, John WG, Mosca A. A Review of the Challenge in Measuring Hemoglobin A1c. J Diabetes Sci Technol. mayo de 2009;3(3):439-45.
- NGSP. Certified Methods and Laboratories [Internet]. Harmonizing Hemoglobin A1c Testing. 2022. Disponible en: http://www.ngsp.org/certified.asp
- NGSP. Obtaining Certification [Internet]. Harmonizing Hemoglobin A1c Testing. 2010. Disponible en: http://www.ngsp.org/critsumm.asp