Helicobacter Pylori detection and elimination
By: Dr. Natalia Loaiza Díaz, M.D.
Medical Microbiologist, Clinical Pathology Leader. Laboratorio Clínico Hematológico S.A.S.
Published: April 25, 2023
The first thing to do is to consult when symptoms of gastritis are present (pain or burning in the upper abdomen, accompanied or not by nausea, vomiting, a feeling of fullness or lack of appetite), when a family member or partner has been informed that he/she has the infection, or in cases of unexplained iron deficiency anemia or idiopathic thrombocytopenic purpura. According to the findings of the physician during the interview and physical examination, he/she will indicate the test that he/she considers pertinent.
Currently, several types of tests are available in the field to approach the diagnosis of this infection. Some of them require gastric tissue obtained by biopsy during digestive endoscopy procedures; therefore, they are considered invasive. Others look for “clues” to the microorganism indirectly, i.e. without reaching the tissue, and are therefore considered non-invasive.
For the results of both groups of tests to be optimal and to avoid false results, it is essential for the patient to stop taking drugs such as antibiotics (four weeks before) and proton pump inhibitors (two weeks before), except for serum (blood) antibody detection tests, which do not require this.
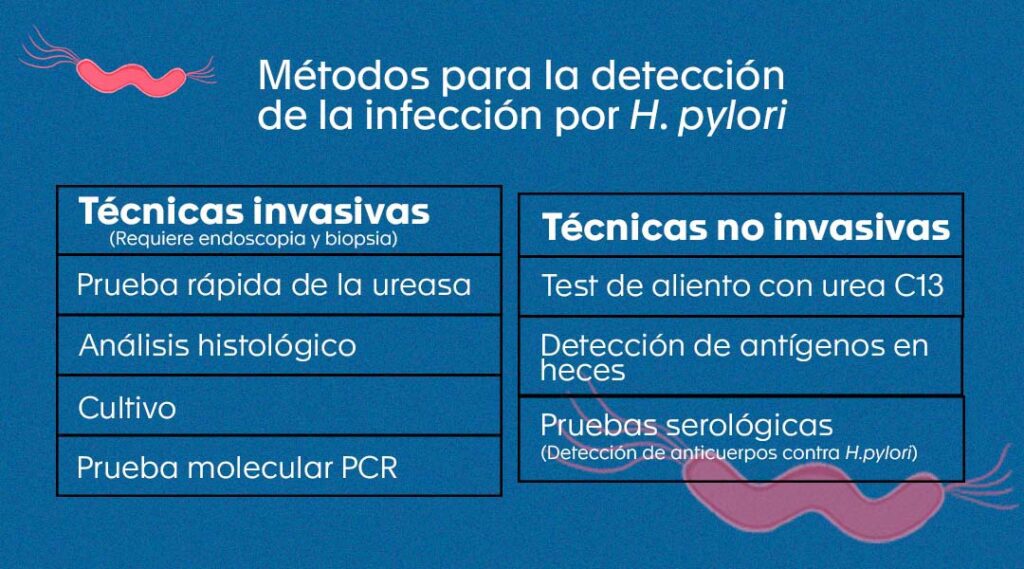
Non-invasive tests:
- Urea breath test 3-6,8,10.
This test is considered the best among the non-invasive methods to make the diagnosis of H. pylori infection and is available at the Hematológico. It is useful both for initial diagnosis and to confirm whether treatment was successful once it has been completed.
The test measures the activity of the urease enzyme produced by the bacteria to establish itself in the stomach. It consists of administering orally to the patient (on an empty stomach) a dilution containing a type of urea labeled with carbon 13 (13C-urea), a non-radioactive isotope of carbon. If H. pylori is present, its enzyme urease will hydrolyze or break down 13C-urea into ammonia and bicarbonate. The latter will be 13C-labeled and will pass into the circulation, travel to the lungs and exit on exhalation as 13C-labeled carbon dioxide (13CO2).
Subsequently, a sample of exhaled air (or breath) is taken from the patient and the 13CO2 released is quantified in comparison to that of a breath sample taken before ingesting the 13C-urea solution, using specialized equipment that allows 13CO2 to be separated from the CO2 that is normally exhaled.
- Detection of H. pylori antigen in fecal material 3-5,8,9,11.
- Detection of IgA, IgM and IgG antibodies against H. pylori 3-5,8,9,11.
This non-invasive technique is available at the Hematológico through allied laboratories and allows us to know if the person has been in contact with the microorganism previously, since it measures immunoglobulin (Ig) antibodies of different classes (IgA, IgM and IgG) produced by the patient’s immune response against H. pylori. The sample used is serum (blood) obtained by venipuncture.
The antibodies measured in this test do not allow differentiation between a past and an active infection, nor does their value relate to the severity of the infection. Furthermore, since they can remain in the blood for more than one year, they should not be used to determine whether the treatment was successful or not.
Invasive tests:
To perform these tests, the patient must first undergo an endoscopy procedure, which is usually performed under sedation. In this, in addition to appreciating with the help of a camera how the stomach mucosa is, biopsies can be taken. What is recommended by the Sydney system, a standardized method used worldwide for the classification of gastritis and the reporting of endoscopic and biopsy findings, in its 1994 updated version, is to take five tissue fragments or biopsies, as follows: two from the antrum, two from the body, and one from the incisura.
The above, with the aim of increasing the probability of detecting the microorganism and of timely detecting premalignant lesions, since the greater the amount of tissue seen under the microscope or sown in culture, the greater the probability of observing H. pylori or obtaining its colonies.
- Histological examination.
- Rapid urease test
- Helicobacter pylori culture
- Molecular tests for H. pylori detection
In the Hematológico.
Bibliography
- Guevara B, Cogdill AG. Helicobacter pylori: A Review of Current Diagnostic and Management Strategies. Dig Dis Sci. julio de 2020;65(7):1917–31
- Organización Panamericana de la Salud. Erradicar la infección por Helicobacter Pylori es todo un reto local y mundial. [Internet]. 2021 [citado el 5 de abril de 2023]. Disponible en: https://www.paho.org/es/noticias/8-3-2021-erradicar-infeccion-por-helicobacter-pylori-es-todo-reto-local-mundial
- Best LM, Takwoingi Y, Siddique S, Selladurai A, Gandhi A, Low B, et al. Non-invasive diagnostic tests for Helicobacter pylori infection. Cochrane Upper GI and Pancreatic Diseases Group, editor. Cochrane Database Syst Rev [Internet]. el 15 de marzo de 2018 [citado el 5 de abril de 2023];2018(3). Disponible en: http://doi.wiley.com/10.1002/14651858.CD012080.pub2
- Chahuan J, Pizarro M, Riquelme A. Métodos diagnósticos para la detección de infección por Helicobacter pylori. ¿Cuál y cuándo deben solicitarse? Acta Gastroenterológica Latinoam [Internet]. el 30 de marzo de 2022 [citado el 5 de abril de 2023];52(1). Disponible en: https://actaojs.org.ar/ojs/index.php/acta/article/view/176
- Diaconu S, Predescu A, Moldoveanu A, Pop CS, Fierbințeanu-Braticevici C. Helicobacter pylori infection: old and new. J Med Life. 2017;10(2):112–7.
- Fischbach W, Malfertheiner P. Helicobacter Pylori Infection. Dtsch Ärztebl Int [Internet]. el 22 de junio de 2018 [citado el 5 de abril de 2023]; Disponible en: https://www.aerzteblatt.de/10.3238/arztebl.2018.0429
- Gallardo Padilla M, León Falconi JL, Sánchez-Nebreda Arias R, Gómez Santos C, Muñoz Egea M del C, la Orden Izquierdo E. Impacto del uso de las técnicas moleculares (PCR) en la detección y el éxito erradicador frente a Helicobacter pylori. An Pediatría. marzo de 2022;96(3):190–5.
- Llorca-Otero L, Toro-Rueda C. Diagnosis of Helicobacter pylori infection: Progress and challenges. Enfermedades Infecc Microbiol Clínica. noviembre de 2020;38(9):407–9.
- Muñoz MS, Valle Rossi ML, Ferrer L, Medeot R, Herrera Najum P, López L, et al. Utilidad del antígeno de Helicobacter pylori en heces como método diagnóstico no invasivo. Acta Gastroenterológica Latinoam. 2019;49(1):22–31.
- Campuzano Maya G. Prueba de aliento optimizada con urea marcada con car-bono 13 para la detección de Helicobacter pylori (PAU-Hp13C®). Med Lab. el 1 de marzo de 2012;18(3–4):137–60.
- Murray PR, Rosenthal KS, Pfaller MA. Medical microbiology. Ninth edition. Edinburgh ; New York: Elsevier; 2021. 855 p.
- Otero R W, Trespalacios R AA, Otero P L, Vallejo O MT, Torres Amaya M, Pardo R, et al. Guía de práctica clínica para el diagnóstico y tratamiento de la infección por Helicobacter pylori en adultos. Rev Colomb Gastroenterol. 2015;30:17–33.
- Sanchez Londoño S, Guevara Casallas G, Niño S, Arteta Cueto A, Marcelo Escobar R, Camilo Ricaurte J, et al. Patrones de detección de Helicobacter pylori y lesiones relacionadas mediante protocolo Sydney en una población de Antioquia, Colombia. Rev Gastroenterol Perú. el 30 de junio de 2022;42(2):86.
- Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol. febrero de 2017;112(2):212–39.
- Owen RJ. Molecular testing for antibiotic resistance in Helicobacter pylori. Gut. el 1 de marzo de 2002;50(3):285–9.
- Matta AJ, Pazos AJ, Bustamante-Rengifo JA, Bravo LE. Genomic variability of Helicobacter pylori isolates of gastric regions from two Colombian populations. World J Gastroenterol. el 7 de febrero de 2017;23(5):800–9.
- Moreno-Flores A, Potel-Alvarellos C, Álvarez-Fernández M. Helicobacter pylori, evolución de la resistencia a antimicrobianos 2012-2020 en el área sanitaria de Vigo, Pontevedra, España. Enfermedades Infecc Microbiol Clínica. diciembre de 2021;39(10):523–4.
- Correa G S, Cardona A AF, Correa G T, Correa L LA, García G HI, Estrada M S. Prevalencia de Helicobacter pylori y características histopatológicas en biopsias gástricas de pacientes con síntomas dispépticos en un centro de referencia de Medellín. Rev Colomb Gastroenterol. 2016;31:9–15.
- Atehortua Rendon JD, Pérez Cala TL, Martínez A. Descripción de la resistencia de Helicobacter pylori a seis antibióticos de uso frecuente en Colombia. Rev Colomb Gastroenterol. el 30 de septiembre de 2020;35(3):351–61.
- de Brito BB, da Silva FAF, Soares AS, Pereira VA, Santos MLC, Sampaio MM, et al. Pathogenesis and clinical management of Helicobacter pylori gastric infection. World J Gastroenterol. el 7 de octubre de 2019;25(37):5578–89.